This preview lesson has been taken from the Online Advanced Herbal Course. The Advanced Herbal Course is made up of 14 Units and 78 Lessons written by some of the most brilliant minds in herbalism. To learn more about the Advanced Herbal Course, please visit the course registration page. We’d love to have you join our Herbal Academy family!
This lesson will introduce you to ways of supporting the endocrine system within the context of a range of endocrine disorders. Each section covers dietary and lifestyle considerations as well as supporting herbs. The aim of the lesson is to give you a broad understanding which you can then integrate into a larger wellness strategy for your client. Throughout this unit you should consider the interconnectedness of different endocrine disorders and the nervous system discussed in Lesson 2 of this unit. This lesson also links with Lesson 4 in which you will learn about different endocrine disorders in more detail. Throughout all of these lessons, and in clinical practice, it is important to develop your critical thinking skills and to support people holistically.
Supporting the nervous system is at the heart of supporting a number of hypothalamic-pituitary disorders. Not only does sustained stress disrupt the hypothalamic-pituitary-adrenal (HPA) axis, but it also impacts the other hypothalamic-pituitary axes (such as the thyroid and growth hormone axes) (Considine, 2013; Pocock & Richards, 2006). Furthermore, as discussed in Lesson 2 of this unit, stress activates the sympathetic nervous system, causing the adrenal glands to release epinephrine, norepinephrine, and glucocorticoids. These are all glucogenic hormones which raise blood glucose levels (Pocock & Richards, 2006).
Relaxation exercises – such as diaphragmatic breathing, visualization, yoga, and meditation – enable a switch from the stress response (in which the sympathetic nervous system dominates) to the relaxation response (in which the parasympathetic nervous system dominates) (Bove et al., 2010; Murray, 2014a).

Exploring hobbies and interests also reduces stress; for example someone who loves art could be encouraged to take up drawing and painting or to join a local art class. Being surrounded by nature (i.e. through walking or gardening) is particularly beneficial. Studies have shown that being in nature (rather than urban environments) helps people to recover from stress more quickly, and that both the sights and sounds of nature have positive effects (Alvarsson et al., 2010; Parsons et al., 1998; Ulrich et al., 1991). Research has also shown that when patients in hospitals are exposed to plants in their rooms they experienced shorter stays, lower heart rate and systolic blood pressure, less pain, need fewer analgesics, and were less anxious and fatigued than those with no plants in their room (Park, 2006; Park & Mattson, 2008). Itis also important that people have adequate social support; those without have reduced life expectancy (Berkman et al., 1992; Rosengren et al., 1993; Rutledge et al., 2004).
Poor sleep affects physical and mental function. Disruption of diurnal sleep patterns (sleeping at night and being awake during the day) can affect hormone secretion – for example, corticosteroid secretion follows a circadian rhythm (Considine, 2013). Establishing good sleep hygiene can be helpful where there are sleep problems – for example, waking up at the same time every day to ensure a sleep-wake rhythm, avoiding caffeine in the evening, ensuring that the bedroom is cool and dark and most importantly a place for sleeping, and relaxing in the evening (Hoffmann, 2003; Murray, 2012). Drinking alcohol affects serotonin levels and releases adrenaline, and can thus affect sleep (Murray, 2012). Regular daily exercise can help to promote sleep providing it is not just before bedtime (Hoffmann, 2003). Ensuring good blood sugar regulation (discussed in depth later) also promotes sleep; a drop in blood sugar levels during the night can cause the person to wake (maintenance insomnia) (Pizzorno et al., 2008).
The adrenal glands need vitamin B5 (Pantothenic acid), vitamin C and folic acid to function properly (Haas, 1992). Meats, vegetables, and cereals are the main sources of vitamin B5. Green leafy vegetables such as chard, spinach, and kale are the best sources of folic acid. Citrus fruits are very high in vitamin C (Barasi, 2003).
Excessive consumption of caffeine can cause symptoms including nervousness, palpitations, insomnia, depression, mood changes, and headaches. Some people, particularly those who are anxious and stressed, are more sensitive to caffeine than others (Murray, 2014a). Furthermore, caffeine causes depletion of B vitamins (Hechtman, 2012).
Exercise increases the production of endorphins which elevate the mood. Exercise also decreases anxiety and malaise, promotes happiness, and can reduce depression (Pizzorno et al., 2008).

Research investigating the gut-brain axis has focused on the impact that the brain has on the gut, for example the impact of stress on functional bowel disorders, such as irritable bowel syndrome (Neufeld & Foster, 2009). Emerging research indicates that the gut-brain axis is bidirectional. For example, a study by Tillisch et al. (2013) investigated the effects of a fermented milk product containing the probiotics Bifidobacterium animalis subsp Lactis, Streptococcus thermophiles, Lactobacillus bulgaricus, and Lactococcus lactis subsp. Lactis in 36 healthy women. The study found that the fermented milk product modulated brain activity, affecting regions of the brain that control the central processing of emotion. A study by Messaoudi et al. (2010) investigated the psychotropic effects on humans of a probiotic formulation containing Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 (PF). Fifty-five healthy participants, exposed to everyday life events, completed the 30-day randomised, double-blind, placebo-controlled, parallel clinical study. The study found that those receiving the probiotic formulation showed beneficial effects in relation to signs of anxiety and depression, and lowered urinary cortisol levels.
A study by Schmidt et al. (2014) investigated the effects of taking prebiotics Bimuno®-galactooligosaccharides (B-GOS) and fructooligosaccharides (FOS) on 45 healthy volunteers. After 3 weeks those who took the B-GOS had lower salivary cortisol levels on waking, and paid more attention to positive words and less attention to negative words compared to placebo (thus B-GOS affected their emotional processing), whereas those who took the prebiotic FOS showed no change to cortisol levels or emotional processing. Animal studies by Savignac et al. (2013) have also indicated that GOS increases proliferation of gut microbiota more than FOS; this may explain why Schmidt et al. (2014) found B-GOS to be more effective than FOS. Schmidt et al. (2014) propose that prebiotics may modulate the HPA axis, and that the positive impact of B-GOS on emotional processing is comparable with the effects of citalopram and diazepam on healthy volunteers.
Although the effects of both prebiotics and probiotics on anxiety and depression warrant further research, the findings so far suggest that promoting healthy gut bacteria should be considered when supporting people with anxiety.
Adaptogens play an important role in increasing the body’s resistance to the negative effects of stress. They help to adapt to stress by supporting the neuroendocrine system and their amphoteric effects help to maintain homeostasis (Winston & Maimes, 2007). Adaptogens normalize the HPA axis by supporting the adrenal glands to both respond to stress and to stop releasing stress hormones when the stressful situation is over. Furthermore, by increasing the sensitivity of the hypothalamic receptors the adrenal glands can release lower levels of stress hormones to achieve the same response (Yance, 2013). Adaptogens that specifically support the adrenal glands include ashwagandha (Withania somnifera), eleuthero (Eleutherococcus senticosus), licorice (Glycyrrhiza glabra), American ginseng (Panax quinquefolius) (for mild to moderate HPA depletion), rhodiola (Rhodiola rosea) and schizandra (Schizandra sinensis). Schizandra, ashwagandha, Asian ginseng, and rhodiola also help to relieve anxiety and depression (Winston & Maimes, 2007).

Ashwagandha is an Ayurvedic herb which has traditionally been used as a restorative, and is thus beneficial for debility and weakness (McIntyre, 2005). It is also a calming and strengthening adaptogen. Coupled with its nervine action, it is valuable for supporting the nervous system and is beneficial for anxiety, stress-induced insomnia and nervous exhaustion (McIntyre, 2005; Winston & Maimes, 2007).
Modern research supports its traditional use. For example, Pratte et al. (2014) conducted a systematic review of randomised controlled trials (in humans) investigating the use of ashwagandha for the treatment of anxiety. All of the 5 trials identified showed that it decreased anxiety. Cooley et al. (2009) conducted a 12-week randomized controlled trial investigating naturopathic care versus psychotherapy for 81 people with anxiety using the Beck Anxiety Inventory (BAI) as its primary outcome measure. All of the participants had experienced more than 6 weeks anxiety prior to the start of the study. Those receiving naturopathic care were given 300 mg twice daily of ashwagandha (standardized to 1.5% withanolides), a multivitamin, dietary counseling, and deep breathing exercise. Those receiving psychotherapy also received deep breathing exercises and placebo. Seventy-five participants completed 8 weeks or more, and the results showed that the group receiving naturopathic care experienced a significant decrease in anxiety compared to those receiving psychotherapy. However, the design of the study compromises its internal validity (true blinding could not be achieved and there was no true control group). Furthermore, as the naturopathic group were given ashwagandha and dietary counseling, the benefits of the herb cannot be clearly established.
Safety: Ashwagandha is rich in iron and therefore should be avoided by those with hemochromatosis (excess iron). It should also be avoided by those sensitive to the nightshade family (Winston & Maimes, 2007). Winston and Maimes (2007) also state that ashwaganda should be avoided by those with hyperthyroidism. Although it has been shown to have thyroid-stimulating properties (Panda & Kar, 1998; 1999), this research was conducted on mice and further in vivo human studies are required in order to ascertain its clinical relevance. According to Mills and Bone (2008) high doses can upset the gastrointestinal system, causing vomiting and diarrhea.
Suggested Usage: Decoction: ½ teaspoon of dried root in 8 ounces of water, decoct for 10 minutes. Drink 4 ounces 3x per day; Tincture: 30-40 drops (equivalent to 1.5-2 mL) (of a 1:5 tincture) 3x/day; Capsule: One 400-500 mg capsule 2x/day.
* Suggested usage information is from Adaptogens: Herbs for strength, stamina, and stress relief by David Winston & Steven Maimes.
In Ayurvedic medicine, ashwagandha powder is added to warm milk or water, decocted with milk, or prepared in ghee. Honey can be used to sweeten the decoction (McIntyre, 2005).
Asian ginseng was traditionally used in Chinese medicine to promote longevity and to “replenish vital energy” (Mills & Bone, 2000), thus it may be best suited for the elderly or the extremely depleted. Traditional Chinese medicine also uses Asian ginseng for insomnia and debility (McIntyre, 1999). According to Mills & Bone (2000), Asian ginseng acts on the HPA axis, increasing vitality and resistance to stress. Likewise, Winston & Maimes (2007) state that Asian ginseng regulates the HPA axis, and is an immune amphoteric (immunomodulator) and a stimulating adaptogen. McIntyre (1999) recommends using Asian ginseng for anxiety, depression, and nervous exhaustion. Studies on rats suggest that Asian ginseng may improve the sensitivity of the HPA axis to cortisol (Head & Kelly, 2009). However, the validity of extrapolating animal studies to humans is questionable. The majority of clinical studies in humans show that Asian ginseng improves physical performance (Mills & Bone, 2000).
 Safety: Asian ginseng should be avoided by those with hypertension and acute infections. Traditionally, Asian ginseng is contraindicated in signs of heat, excessive nose bleeds or menstruation, acute asthma, and signs of heat. It may also cause overstimulation in susceptible individuals (particularly when taking higher doses) (Mills & Bone, 2000). Those with anxiety, insomnia or hypertension should avoid high doses and concomitant intake of caffeine or other stimulants (Mills & Bone, 2000; Winston & Maimes, 2007). Those taking monoamine oxidase inhibitors and warfarin should avoid taking Asian ginseng (Mills & Bone, 2000).
Safety: Asian ginseng should be avoided by those with hypertension and acute infections. Traditionally, Asian ginseng is contraindicated in signs of heat, excessive nose bleeds or menstruation, acute asthma, and signs of heat. It may also cause overstimulation in susceptible individuals (particularly when taking higher doses) (Mills & Bone, 2000). Those with anxiety, insomnia or hypertension should avoid high doses and concomitant intake of caffeine or other stimulants (Mills & Bone, 2000; Winston & Maimes, 2007). Those taking monoamine oxidase inhibitors and warfarin should avoid taking Asian ginseng (Mills & Bone, 2000).
Suggested Usage: Decoction: ½ teaspoon of powdered root to 1 cup of water. Bring to the boil and gently simmer for 10 minutes. Drink 3x/day; Tincture: 1-2 mL (1:5 tincture in 60% alcohol) 3x/day; Powdered Extract: One 400-500 mg capsule 2x/day.
*Suggested usage information is from Medical Herbalism: The science and practice of herbal medicine by David Hoffmann, and Adaptogens: Herbs for strength, stamina, and stress relief by David Winston & Steven Maimes.
Eleuthero (sometimes called Siberian ginseng) is a mild adaptogen which helps the body to withstand and adapt to stress; eleuthero is indicated for stressed-out, over-worked people (Winston & Maimes, 2007). Its nervine action helps to promote restful sleep. Eleuthero is milder and less stimulating than Asian ginseng (Mills & Bone, 2010; Winston & Maimes, 2007).
 Research investigating the effects of eleuthero on endurance capacity has shown mixed results. A double-blind randomized, placebo-controlled, crossover trial with a four week washout period conducted by Kuo et al. (2010) found that eleuthero increased endurance capacity. However, other well-designed studies have found eleuthero to have no effect on exercise endurance (Dowling et al.,1996; Eschbach et al., 2000). Gaffney et al. (2001) investigated the effects of eleuthero and Asian ginseng on athletes. 30 athletes received either 8 mL/day of extract (equivalent to 4g/day) of Eleuthero, 4 mL/day of extract (equivalent to 2g/day) of Asian ginseng (topped up to 8mL with water and drinking ethanol), or a placebo for a six week period. Eleuthero was shown to significantly decrease testosterone:cortisol ratio (by increasing cortisol levels). According to the authors this is in line with animal studies which suggest that eleuthero increases the stress response when stress is below a threshold, and decreases the stress response when above. Thus the stress experienced by the athletes may have been below the hypothetical threshold. However, further research is needed to confirm this theory. Panax ginseng did not affect cortisol or testosterone levels.
Research investigating the effects of eleuthero on endurance capacity has shown mixed results. A double-blind randomized, placebo-controlled, crossover trial with a four week washout period conducted by Kuo et al. (2010) found that eleuthero increased endurance capacity. However, other well-designed studies have found eleuthero to have no effect on exercise endurance (Dowling et al.,1996; Eschbach et al., 2000). Gaffney et al. (2001) investigated the effects of eleuthero and Asian ginseng on athletes. 30 athletes received either 8 mL/day of extract (equivalent to 4g/day) of Eleuthero, 4 mL/day of extract (equivalent to 2g/day) of Asian ginseng (topped up to 8mL with water and drinking ethanol), or a placebo for a six week period. Eleuthero was shown to significantly decrease testosterone:cortisol ratio (by increasing cortisol levels). According to the authors this is in line with animal studies which suggest that eleuthero increases the stress response when stress is below a threshold, and decreases the stress response when above. Thus the stress experienced by the athletes may have been below the hypothetical threshold. However, further research is needed to confirm this theory. Panax ginseng did not affect cortisol or testosterone levels.
Safety: Eleuthero is contraindicated during the acute phase of infections. It is recommended that it should only be taken for 6 weeks, and then followed by a break for 2 weeks. A few cases have reported that eleuthero caused insomnia, pericardial pain, hypertension, and tachycardia in those with cardiovascular disorders. Exceeding normal dose increases the likelihood of side effects (Mills & Bone, 2008). As with all herbal medicines, ensure that eleuthero is purchased from a reputable company – eleuthero has been known to be adulterated with Periploca sepium, which contains cardiac glycosides and may have been the cause of toxicity attributed to eleuthero (Winston & Maimes, 2007).
Suggested Usage: Decoction: 1-2 teaspoons powdered dried root in 12-16 ounces of water. Slowly decoct for 20-30 minutes and then steep for 1 hour. Drink up to 3 cups per day; Tincture: 60-100 drops (equivalent to 3-5 mL) (of a 1:4 tincture), 3-4 x/day.
*Suggested usage information is from Adaptogens: Herbs for strength, stamina, and stress relief by David Winston & Steven Maimes.
Nervines can be used alongside adaptogens to complement their effects on the nervous system. Some adaptogens, such as ashwagandha, schizandra, eleuthero, and rhodiola are also nervines (Winston & Maimes, 2007). Nerve tonics and relaxing nervines are indicated for supporting anxiety and stress.
Nerve tonics strengthen and feed the nervous system (Hoffmann, 1997). Milky oats (Avena sativa), skullcap (Scutellaria laterifolia), damiana (Turnera diffusa), St. John’s wort (Hypericum perforatum), vervain (Verbena officinalis) and wood betony (Stachys betonica) are examples of nerve tonics (Bartram, 1998; Hoffmann, 1997). Relaxing nervines can be used to ease anxiety and tension; examples include linden (Tilia spp.), passionflower (Passiflora incarnata), lavender (Lavendula angustifolia), valerian (Valeriana officinalis), and motherwort (Leonurus cardiaca). St. John’s wort and lemon balm (Melissa officinalis) are nervines which have an uplifting and anti-depressant effect (Hoffmann, 1997; Winston & Maimes, 2007).
 Milky oats are a nutritious herb which is both relaxing and stimulating (McIntyre, 1999). It is the best example of a nervous trophorestorative – being high in vitamins and minerals, it strengthens and nourishes the nervous system and is considered food for the nerves. It is therefore indicated for nervous exhaustion, fatigue, weakness and depression (Hoffmann, 1997; McIntyre, 1999; Winston & Maimes, 2007). Winston and Maimes (2007) advocate using a fresh tincture or glycerite made from the immature seed collected when they are filled with a milky sap. According to mcdonald (n.d.), milky oats also support the adrenal glands. Taken over a period of time they strengthen the nervous system, supporting the person to both physically and mentally cope better.
Milky oats are a nutritious herb which is both relaxing and stimulating (McIntyre, 1999). It is the best example of a nervous trophorestorative – being high in vitamins and minerals, it strengthens and nourishes the nervous system and is considered food for the nerves. It is therefore indicated for nervous exhaustion, fatigue, weakness and depression (Hoffmann, 1997; McIntyre, 1999; Winston & Maimes, 2007). Winston and Maimes (2007) advocate using a fresh tincture or glycerite made from the immature seed collected when they are filled with a milky sap. According to mcdonald (n.d.), milky oats also support the adrenal glands. Taken over a period of time they strengthen the nervous system, supporting the person to both physically and mentally cope better.
Oatstraw (the entire grass) is a nutritive tonic, rich in minerals such as calcium and magnesium. It is best taken as a strong infusion (steeped for several hours) (mcdonald, n.d.). Oats can also be eaten as oatmeal, and like oatstraw are a nutritive tonic (a good source of B vitamins and minerals). Both support the nervous system and are mildly anti-depressant (Chevallier, 1996).
Safety: Those with celiac disease (gluten intolerance) should avoid (Winston & Maimes, 2007). However, it is worth noting that oats themselves do not contain gluten – rather the concern stems from cross-contamination with gluten-containing cereals (National Health Service [NHS], 2014).
Suggested Usage: Infusion: 1-3 teaspoons of dried oatstraw to one cup of boiling water. Infuse for 10-15 minutes and drink 3x/day. Tincture: 3-5 mL of oatstraw (1:5 tincture in 25% alcohol) 3x/day, and 80-100 drops (equivalent to 4-5 mL) of fresh milky oat immature seed (1:2 tincture) 3-4x/day.
*All suggested usage information is from Medical herbalism: The science and practice of herbal medicine by David Hoffmann, and Adaptogens: Herbs for strength, stamina, and stress relief by David Winston & Steven Maimes.
 Skullcap was used as a nerve tonic and sedative in North American folk medicine. The Eclectic physicians used it for nervousness caused by physical and mental exhaustion and illness, and functional cardiac disorders caused by anxiety (Felter & Lloyd, 1898). Skullcap is used by modern herbalists to help relieve stress and reduce anxiety, to relieve tension headaches, insomnia, and for nervous exhaustion (Bartram, 1998; McIntyre, 1999). It is also a good source of minerals (McIntyre, 1999).
Skullcap was used as a nerve tonic and sedative in North American folk medicine. The Eclectic physicians used it for nervousness caused by physical and mental exhaustion and illness, and functional cardiac disorders caused by anxiety (Felter & Lloyd, 1898). Skullcap is used by modern herbalists to help relieve stress and reduce anxiety, to relieve tension headaches, insomnia, and for nervous exhaustion (Bartram, 1998; McIntyre, 1999). It is also a good source of minerals (McIntyre, 1999).
A study by Wolfson & Hoffmann (2003) suggests that skullcap may be beneficial for anxiety. They conducted a double-blind, placebo-controlled cross-over trial investigating the anxiolytic effects of skullcap. 19 healthy volunteers took 4 one-off treatments – placebo, 100 mg, 200 mg and 350 mg capsule of organic freeze dried Scutellaria lateriflora (different producers) – staggered with 2 days intervals. Anxiety, cognition, and energy were measured at baseline, and at 30, 60, 90, and 120 mins after administration. The results showed that all of the preparations of skullcap had a positive effect on anxiety compared to the placebo. However, the study design was methodologically poor, and insufficient reporting makes determining the statistical significance of the results difficult.
Brock et al. (2014) conducted a randomised, double-blind, placebo-controlled crossover study investigating the effects of Scutellaria lateriflora on mood. This was on the whole a well-designed study in which 43 healthy volunteers were given either skullcap (350 mg three times a day), or placebo for a two-week period. This was followed by a 7 day wash-out period, before receiving the other preparation. The results showed that there was no significant difference between the placebo and skullcap for reducing anxiety (Beck anxiety inventory score). However, it is worth noting that at the start of the study 81% of the volunteers were mildly anxious (or less), thus the results are of little surprise. Future research should investigate the anxiolytic effects of skullcap on notable anxious populations.
Safety: No safety concerns based on current evidence (Mills & Bone, 2008).
Suggested Usage: Infusion: 1-2 teaspoons of dried herb per cup of boiling water. Infuse for 10-15 minutes and drink 1 cup 3x/day, or when needed; Tincture: 60-80 drops (equivalent to 3-4 mL) (1:2 fresh herb tincture) up to 4x/day.
*Suggested usage information is from Adaptogens: Herbs for strength, stamina, and stress relief by David Winston & Steven Maimes, and The Holistic Herbal by David Hoffmann.
Lemon balm is an uplifting nervine, beneficial for when depression or anxiety affects the heart and causes symptoms such as palpitations (McIntyre, 1999). It is indicated for stress headaches and to aid sleep (Winston & Maimes, 2007). Lemon balm is also a carminative, and is particularly indicated for digestive issues accompanied with emotional problems or stress. Lemon balm tea is best when fresh leaves are used, and ensure it is covered when infusing to prevent the loss of beneficial essential oils (Chevallier, 1994). Kennedy et al. (2004) investigated the effects of lemon balm on laboratory-induced psychological stress in 18 healthy volunteers using a double-blind, placebo-controlled, randomized, crossover trial. 600 mg of lemon balm reduced the negative effects of the psychological stress. 
Safety: None required on current evidence (Mills & Bone, 2000). According to Hoffmann (2003) lemon balm may interfere with thyroid hormones. However (as discussed later in this lesson), this recommendation is questionable.
Suggested Usage: Infusion: 2-3 teaspoons of the dried herb to 1 cup of boiling water, cover and infuse for 10-15 minutes. Drink morning and evening, or when needed; Tincture: 2-6 mL (1:5 tincture in 40% alcohol) 3x/day.
*Suggested usage information is from Medical herbalism: The science and practice of herbal medicine by David Hoffmann.
Goitrogens can block the synthesis of thyroid hormones by inhibiting the uptake of iodine, interfere with the organification of iodide, or affect the release of thyroid hormones (Gropper & Smith, 2012). A number of foods, pharmaceutical drugs and environmental pollutants have been identified as being goitrogenic (see Table 1). Furthermore, some pharmaceuticals (carbamazepine, phenytoin, phenobarbitone, and rifampin) also cause metabolic degraduation of T4 and T3. Amiodarone and propylthiouracil inhibit the conversion of T4 to the more potent T3 (Tripathi, 2013).

| Table 1: Examples of Goitrogenic Substances | ||
| Source | Examples | Notes |
| Foods | Cruciferous vegetables (Brassica family), i.e. cabbage, kale, turnips, broccoli and rapeseed – contain glucosinolates. Metabolites of glucosinolates compete with iodine (Zimmermann, 2012) | Cooking/heating these foods renders them inactive (Murray & Pizzorno, 1990a) |
| Lima beans, cassava, sweet potato and linseed contain cyanogenic glucosides which may be metabolized to thiocynates (Zimmermann, 2012). Cassava contains the cyanogenic glucoside linaramin which is converted to thiocyanate (which competes with iodine for thyroidal uptake) (Gropper & Smith, 2012; Zimmermann, 2012) | Soaking and cooking cassava removes the linaramin (Zimmermann, 2012). | |
| Soy and millet – may be goitrogenic (Zimmermann, 2012). | ||
| Medications | Lithium inhibits the release of thyroid hormones; thionamides including methimazole, carbomazole and propylthiouracil (antithyroid medication), aminoglutethimide (an antiadrenal medication which inhibits iodide organification), carbutimide, amiodarane (an antiarrhythmic medication – effect is mainly due to iodine content) (Davis & Davis, 2001; Tripathi, 2013; Zimmermann, 2012). | |
| Environmental |
Some humic substances (components of organic matter) in drinking water are goitrogenic. Geology and geochemistry affects the concentration and characteristics of humic substances (Anderson & Laurberg, 2009). | Both humic substances and iodine are found in drinking water (Anderson & Laurberg, 2009). |
| Perchlorate (a drinking water contaminant) (Gropper & Smith, 2012). | ||
Stress disrupts the hypothalamic-pituitary-thyroid (HPT) axis, reducing the production of thyroid hormones. Furthermore, the peripheral conversion of the inactive T4 to the active T3 can be inhibited by glucocorticoids (Andrews et al., 2015). Stress can also cause immune dysregulation and thus autoimmune conditions (Bone, 1994; Mizokami et al., 2004); it is known to trigger Grave’s disease (Longmore et al., 2014; Murray & Pizzorno, 1999a) and possibly Hashimoto’s thyroiditis. However, given the insidious nature of the latter, this is harder to establish. Stress reduction techniques, such as those discussed earlier in this lesson, can be effective in supporting thyroid health.
As well as helping to maintain a healthy weight, exercise stimulates the thyroid to secrete thyroid hormones and increases the sensitivity of tissues to thyroid hormones (Pizzorno et al., 2008).
Zinc and vitamins A, E, B2 (riboflavin), B3 (niacin), and B6 (pyridoxine) are all needed for the synthesis of thyroid hormones (Murray & Pizzorno, 1999a). Sources of zinc include oysters, yeast, eggs, beef, herring, seeds, fruit, nuts, peas, shellfish, and poultry. Sources of vitamin A include fish oils, liver, organic milk, and egg yolks. Yellow and orange colored fruit and vegetables are a good source of carotenoids (provitamin A), which are converted to retinol (a form of vitamin A) (Barasi, 2003; Haas, 1992). To maintain a healthy thyroid, adequate but not excessive amounts of vitamin A should be taken as large amounts can inhibit thyroid function (Pizzorno et al., 2008). Furthermore, toxicity can occur through excessive consumption (usually occurring through supplementing, though it can occur through excessive consumption of liver) (Haas, 1992). Eggs, meat and brewer’s yeast are good sources of vitamins B2, B5, and B6 (McIntyre, 1999).
Selenium, zinc, and copper are required for the conversion of T4 to T3 (Pizzorno et al., 2008). Brazil nuts, garlic, brewer’s yeast, and whole grains contain selenium. Organ meats (i.e. liver), green leafy vegetables, whole grains, eggs, beans, nuts, and seafood are sources of copper (McIntyre, 1999; Pizzorno et al., 2008). In hyperthyroidism, antioxidants such as vitamin C and E are also needed to protect from oxidative damage (caused by elevated thyroid hormones). Furthermore, hyperthyroidism affects calcium metabolism, increasing the risk of osteoporosis (Pizzorno et al., 2008).

Ensuring an adequate – but not excessive – intake of iodine is important as it is needed for thyroid hormone synthesis. The recommended daily allowance of iodine for adults is 150 μg/day (Whitney & Rolfes, 2013). According to Nussey & Whitehead (2001) the thyroid uses 125 μg/day for thyroid hormone synthesis. In chronic states of iodine deficiency the thyroid gland enlarges in an attempt to accumulate more iodine from the blood and thus increases the synthesis of T3 and T4 (Andrews et al., 2015). Iodine deficiency is rare in the United States and Canada (due to iodized salt), though is the most common form of iodine deficiency worldwide (Axford & O’Callaghan, 2004; Vanderpump, 2011). It is worth noting that too much iodine can inhibit the synthesis of thyroid hormones, and thus exacerbate hypothyroidism (Murray & Pizzorno, 1999a) – given this, supplements should be avoided unless iodine deficiency is the cause. Sources of iodine include sea vegetables (such as kelp), sea fish, and iodized salt (Murray & Pizzorno, 1999a).
There is a distinct lack of research investigating the use of herbs for hypothyroidism (Bove et al., 2010). According to Winston and Maimes (2007), rhodiola, ashwagandha and holy basil (Ocimum sanctum) are indicated for hypothyroidism. Rhodiola supports thyroid function but does not cause hyperthyroidism. As adaptogens, they have the additional benefit of helping to regulate the hypothalamic axis and reduce oxidative stress (seen in both hypo- and hyperthyroidism) (Bove et al., 2010). Ashwagandha has been shown to have thyroid-stimulating activity in mice (Panda & Kar, 1998; 1999). However, there is a distinct lack of research investigating the effects in humans. Coleus (Coleus forkohlii) and guggul (Commiphora mukul) are also indicated for hypothyroidism (Bone & Mills, 2013).
 Bladderwrack has traditionally been used for underactive thyroid, obesity and lymphadenoid goiter (Mills & Bone, 2008). Bladderwrack contains organic-bound iodine, which has a greater stimulating effect than mineral-bound iodine (Mills and Bone, 2013). As discussed in lesson 4, iodine deficiency is a known cause of hypothyroidism. However, given that the majority of cases of hypothyroidism in developed countries are autoimmune, it may not be an appropriate choice for all cases.
Bladderwrack has traditionally been used for underactive thyroid, obesity and lymphadenoid goiter (Mills & Bone, 2008). Bladderwrack contains organic-bound iodine, which has a greater stimulating effect than mineral-bound iodine (Mills and Bone, 2013). As discussed in lesson 4, iodine deficiency is a known cause of hypothyroidism. However, given that the majority of cases of hypothyroidism in developed countries are autoimmune, it may not be an appropriate choice for all cases.
Safety: Bladderwrack is contra-indicated in hyperthyroidism. Caution should be exercised during pregnancy and lactation. Those with hypothyroidism taking Bladderwrack should be carefully monitored for signs of hyperthyroidism (Mills & Bone, 2008). Furthermore, care needs to be taken as long term use of a high dose can worsen hypothyroidism (Bone & Mills, 2013). Bladderwrack may also interfere with thyroid replacement therapies (Bove et al., 2010). Source bladderwrack which has been grown in an environment free of heavy metals (Mills & Bone, 2013).
Suggested Usage: INFUSION: 2-3 teaspoon of the dried herb per cup of boiling water. Infuse for 10 minutes and drink 3x/day; TINCTURE: 4-10 mL/day (of a 1:5 tincture).
* All suggested usage information is from The holistic herbal by David Hoffmann and The essential guide to herbal safety by Simon Mills and Kerry Bone.
There are a number of herbs which are considered to have anti-thyroid activity, for example bugleweed (Lycopus virginicus/europaeus), lemon balm, motherwort and gromwell (Lithospermum officinale) (Bove et al., 2010).
Modern herbalists use motherwort to support people with hyperthyroidism (Bartram, 1998; Bove et al., 2010; Hoffmann, 2003). It is a cardiotonic which is particularly indicated for palpitations and rapid heartbeat associated with anxiety and hyperthyroidism (Chevallier, 2008; Hoffmann, 1997; McIntyre, 1999). A lack of research investigating the effect of motherwort on thyroid function makes it hard to determine whether it only offers symptomatic relief, or whether it has also has anti-thyroid activity as well.
According to Mills & Bone (2008), lemon balm is a TSH antagonist. Although they do not advocate that it should be avoided/used cautiously in hypothyroidism, a number of other authors do (Braun & Cohen, 2015; Hoffmann, 2003; Winston & Maimes, 2007). Lemon balm is an uplifting nervine, beneficial for when depression or anxiety affects the heart and causes symptoms such as palpitations (McIntyre, 1999), thus offering relief for some of the symptoms of hyperthyroidism. In vitro research suggests that lemon balm has anti-thyroid properties (Auf’mkolk et al., 1984; Auf’mkolk et al., 1985), However, extrapolating the results from this in vitro research to effects in living human beings is impossible. To date there are no studies investigating the effects of lemon balm on thyroid levels in humans, therefore further research in this area is needed before making claims about its effect on the thyroid. However, given its nervine action, using lemon balm in conjunction with bugleweed is recommended.
Bugleweed is a key herb for hyperthyroidism and is particularly indicated when there is shaking, palpitations, tachycardia, and shortness of breath (Bartram, 1998; Hoffmann, 2003). The Eclectic physicians used bugleweed for restlessness, anxiety, insomnia, tachycardia, and exopthalamic goiter (Ellingwood, 1919; Felter & Lloyd, 1898).
In vivo studies have found that injecting Lycopus spp. into animals inhibits TSH and reduces pituitary and serum TSH (Kemper et al., 1961, cited in Mills & Bone, 2013; Winterhoff et al.,1983 cited in Mills & Bone, 2013). A study by by Winterhoff et al. (1994) in which bugleweed was orally administered to rats found that it decreased T3, T4, and TSH levels. However, a study by Vonhoff et al. (2006) found that intraperitoneal injection (injecting into the peritoneum) of bugleweed in rats with induced hyperthyroidism only ameliorated the cardiac symptoms of hyperthyroidism, and did not affect the levels of TSH or thyroid hormones. Thus the effects of Lycopus spp. on the thyroid status of animals is inconclusive. Nevertheless, extrapolating the results to humans is questionable, never mind the issue of injecting bugleweed rather than consuming it as a traditional herbal preparation.

One study (in English) investigating the effects of bugleweed in humans was found (Beer et al., 2008). This study cites others – however, these are in German thus the rigor and validity of these studies cannot be determined. According to Beer et al. (2008), these studies did not show any significant changes on thyroid parameters.
Beer et al. (2008) conducted a prospective two-armed open study investigating its effects on thyroidal parameters and symptoms associated with thyroid function. Sixty-two participants completed the study, and samples of urine from 58 participants were analyzed (although 23 of these were excluded). Bugleweed significantly increased T4 excretion in the urine (T3 excretion was not affected) and improved symptoms. However, the inclusion criteria failed to distinguish between different types of hyperthyroidism, there was no placebo, and it is hard to determine the significance of the results from the writeup of the study. Given the lack of available research investigating the effects of bugleweed in people with hyperthyroidism, the justification for its use stems from traditional knowledge.
Safety: Bugleweed is contraindicated in hypothyroidism, goiter without functional disorder, and during pregnancy and lactation. Caution should also be exercised in women trying to conceive. It should also not be taken alongside preparations containing thyroid hormone, or while under investigation where radioactive isotopes are used (as it can interfere with uptake). In rare cases, high doses and extended use has caused thyroid enlargement (Mills & Bone, 2008).
Suggested Usage: Infusion: 1 teaspoon dried herb to 1 cup of boiling water. Infuse for 10-15 minutes and drink 3x/day; Tincture: 1-2 mL (1:5 tincture in 40% alcohol) 3x/day.
*Suggested usage information is from Medical herbalism: The science and practice of herbal medicine by David Hoffmann.
Insulin resistance can not only lead to type 2 diabetes mellitus and metabolic syndrome, it is seen in polycystic ovary syndrome (PCOS) and has been linked to other diseases such as Alzheimer’s disease, some cancers, and non-alcoholic steatorrhea hepatitis (NASH) (Bone & Mills, 2013). In the case of PCOS, insulin resistance is estimated to affect around 50-70% of women with the condition. Raised levels of circulating insulin increase the production of androgens (Trickey, 2003). Thus regulating blood sugar levels can play a significant role in both the prevention and support of PCOS (this condition will be discussed in greater depth in Unit 7: Female Health and Wellness). Good blood sugar control significantly reduces the likelihood of complications of hyperglycaemia (Murray & Pizzorno, 1999b). Attention should also be given to minimizing factors that disrupt the body’s ability to maintain blood sugar homeostasis, such as elevated cortisol levels. We will be having more in-depth discussions on sugar metabolism in the following lesson, as well as in Unit 10: Weight Management for Health and Wellness.
To help maintain blood sugar regulation, sugars should be consumed in limited amounts as they cause a rapid increase in blood sugar levels and thus elevated insulin levels (Murray, 2014b). Blood sugar spikes compromise the homeostatic mechanisms which regulate blood sugar levels. An ecologic analysis by Gross et al. (2004) found that type 2 diabetes mellitus was strongly associated with an increased consumption of refined carbohydrates and a low consumption of dietary fiber. Foods with a low glycemic index (GI) (e.g., oats, lentils and beans) are broken down more slowly than those with a high GI (e.g., white bread) – thus they raise blood sugar levels more slowly and consequently less insulin is released (Thomas & Elliott, 2009). Many alternatives to refined carbohydrates and sugar, especially within the context of weight management, will be discussed in further detail in Unit 10: Weight Management for Health and Wellness.

Eating a diet high in fiber improves insulin sensitivity (Weickert & Pfeiffer, 2008). Good sources of water-soluble fiber are legumes, oat bran, nuts, seeds, psyllium seed husks, pears, apples, and most vegetables (Pizzorno et al., 2008).
Regular exercise improves insulin sensitivity and helps maintain a healthy body weight (Bone & Mills, 2013). For people who are overweight, sensible weight loss reduces insulin resistance (Hechtman, 2012). We will be discussing weight management for health and wellness in Unit 10.
Raised adrenaline and cortisol levels increase blood glucose levels and insulin resistance (Hechtman, 2012), thus stress management techniques are beneficial for helping to maintain blood sugar regulation and for those with diabetes mellitus (by reducing the impact of stress on blood sugar regulation). Furthermore, those with diabetes are more prone to depression (both before and after onset) and can find living with diabetes challenging (Banasik, 2013). Stress reduction techniques, such as those discussed earlier in this lesson, can be helpful. Obtaining adequate sleep is important for regulating blood sugar levels (Pizzorno et al., 2008).

Epidemiological studies show that low dietary intake of magnesium increases the risk of developing type 2 diabetes (Emoto & Nishizawa, 2007). Studies have also shown that magnesium increases insulin sensitivity in people with type 2 diabetes (Stargrove et al., 2008). Stargrove et al. (2008) recommend a dose of 200-600 mg of elemental magnesium per day for diabetics. It is recommended that magnesium status and kidney function are assessed prior to supplementing. Furthermore, insulin levels need to be regularly monitored. Dietary sources of magnesium include brewer’s yeast, buckwheat, wheat bran, and nuts (cashews, brazil nuts, and almonds). Magnesium deficiency can result from taking a number of pharmaceutical drugs, in particular furosemide, aminoglycosides, and amphotericin-B (Stargrove et al., 2008).
Chromium is important for ensuring blood glucose homeostasis – it activates insulin receptor kinase, increases insulin sensitivity and binding, increases insulin receptor numbers, and promotes glucose uptake. In addition, chromium may lower low-density (LDL) and raise high-density (HDL) cholesterol levels (Stargrove et al., 2008). Dietary sources of chromium include Brewer’s yeast, liver, beef, whole grains, molasses, and wheat germ (Haas, 1992; McIntyre, 1999). However, chromium is difficult to absorb (this worsens with age) and low levels of chromium in modern day soils increase the likelihood of deficiency. Furthermore, refined foods, high in sugars and fats, often contain low levels of chromium (Haas, 1992).
Those who are diabetic and/or insulin resistant can supplement with antioxidants (i.e. vitamin E) to improve insulin sensitivity (Trickey, 2003). Dietary sources of vitamin E include cold-pressed oils (particularly wheat germ oil), nuts, grains, and sprouted seeds (Stargrove et al., 2008).
A number of herbs are indicated for regulating blood sugar levels. These include goat’s rue (Galega officinalis), gymnema (Gymnema sylvestre), and fenugreek (Trigonella foenum-graecum) (Mills & Bone, 2008). We will be revisiting some of these herbs in Unit 10: Weight Management for Health and Wellness. Adaptogens are beneficial for helping the body to cope with and respond to stress, and are therefore indicated for assisting in blood sugar regulation. Key adaptogens which help to regulate blood sugar levels include holy basil, eleuthero, and American ginseng (Panax quinquefolius). Clinical studies support the use of holy basil for reducing blood sugar levels in people with type 2 diabetes mellitus (Winston & Maimes, 2007). Shishtar et al. (2014) conducted a systematic review and meta-analysis of randomized-controlled trials investigating the effect of ginseng (Panax spp.) on glycemic control. 16 studies met the inclusion criteria (12 of these investigated Panax ginseng, 3 investigated American ginseng and 1 was unspecified). The review found that Panax spp. significantly improved fasting blood glucose levels in those with diabetes (and to a lesser degree in those without diabetes). However, larger and longer randomized controlled trials are needed to substantiate these findings.
Gymnema is a key herb that has been traditionally used for diabetes (Bone & Mills, 2013). The common name of ‘gumar’ means ‘sweet destroyer’ – this comes from its ability to temporarily hinder the person’s ability to taste sweetness (Bone & Mills, 2013; Pole, 2013). According to Pole (2013) Gymnema increases the production of insulin by the pancreas and helps to regulate blood sugar levels.
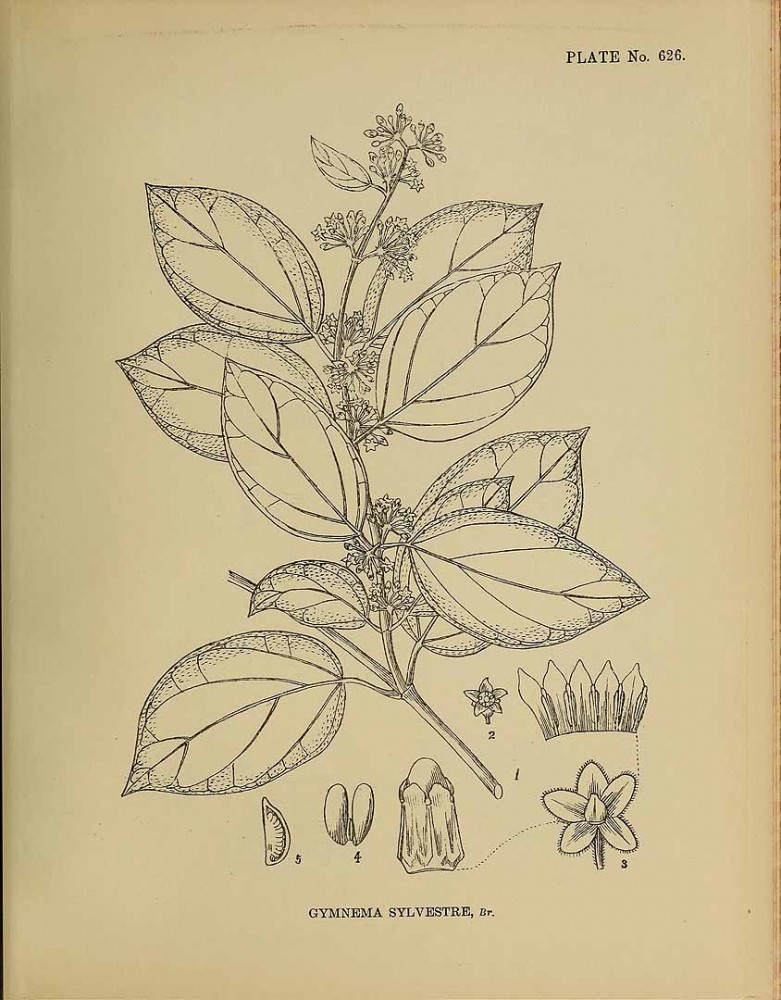 A study by Baskaran et al. (1990) investigated the effectiveness of a leaf extract of Gymnema in 22 type 2 diabetes mellitus volunteers taking conventional oral hypoglycaemic medication. The Gymnema preparation was given alongside conventional medicine for 18-20 months. The results showed that it significantly reduced blood glucose levels, increased fasting and postprandial serum insulin levels, and that hypoglycaemic medication could be reduced. By the end of the study period, 5 of the volunteers were able to regulate their blood glucose levels taking the Gymnema preparation without the need for conventional medication.
A study by Baskaran et al. (1990) investigated the effectiveness of a leaf extract of Gymnema in 22 type 2 diabetes mellitus volunteers taking conventional oral hypoglycaemic medication. The Gymnema preparation was given alongside conventional medicine for 18-20 months. The results showed that it significantly reduced blood glucose levels, increased fasting and postprandial serum insulin levels, and that hypoglycaemic medication could be reduced. By the end of the study period, 5 of the volunteers were able to regulate their blood glucose levels taking the Gymnema preparation without the need for conventional medication.
Shanmugasundaram et al. (1990) investigated the leaf extract of Gymnema (400 mg/day) in 27 volunteers with insulin-dependent diabetes mellitus for 6-30 months. The results suggested that the preparation improved the production of endogenous insulin. They propose that this may have been caused by pancreatic regeneration.
Safety: Gymnema should be used cautiously in those taking hypoglycaemic drugs and insulin – blood sugars levels need to be regularly monitored and the person should be made aware that they may experience hypoglycemia. Because gymnema is rich in saponins, caution should be exercised in those with cholestasis. Furthermore, it may not be suitable for those with celiac disease, vitamin A, D, E and K deficiency, fat malabsorption, and some upper digestive irritations (Mills & Bone, 2008).
Suggested Usage: Infusion: 6-60 g/day of dried leaf; Tincture: 3.5-11 mL/day (1:1 liquid extract).
* Suggested usage information is from The essential guide to herbal safety by Simon Mills & Kerry Bone.
Reducing stress (physiological and psychological), eating a balanced and varied diet rich in whole foods, obtaining adequate sleep, reducing stimulants, and partaking in regular exercise are important for the endocrine system. When supporting people whose endocrine system is out of balance, it is vital to think holistically about what could have contributed to the development of the condition. It is also important to make recommendations that are achievable. Educating your client about dietary and lifestyle factors in a non-judgmental manner can help them to see the importance of making changes and thus increase adherence.
Adaptogens: Herbs for Strength, Stamina, and Stress Relief by David Winston and Steven Maimes
Adaptogens in Medical Herbalism by Donald Yance
The Clinician’s Handbook of Natural Medicine by Joseph Pizzorno, Michael Murray and Herb Joiner-Bey
Alvarsson, J.J., Wiens, S., & Nilsson, M.E. (2010). Stress recovery during exposure to nature sound and environmental noise. International Journal of Environmental Research & Public Health, 7(3), 1036-1046. doi: 10.3390/ijerph7031036 Anderson, S., & Laurberg, P. (2009). The nature of iodine in drinking water. In: Preedy, V.R., Burrow, G.N., & Watson, R.R. (Eds.), Comprehensive handbook of iodine: Nutritional, biochemical, pathological and therapeutic aspects (pp. 125-134). Oxford, UK: Elsevier. Andrews, C., Morgan, M., & Hadfield, R. (2015). Nutritional and herbal support for health adrenal and thyroid function [Mediherb member site]. A Phytotherapist’s Perspective, 196, 1-4. Auf’mkolk, M., Ingbar, J.C., Kubota, K., Amir, S.M., & Ingbar, S.H. (1985). Extracts and auto-oxidized constituents of certain plants inhibit the receptor-binding and the biological activity of Graves’ immunoglobulins. Endocrinology, 116(5), 1687-93. Auf’mkolk, M., Köhrle, J., Gumbinger, H., Winterhoff, H., & Hesch, R.D. (1984). Antihormonal effects of plant extracts: Iodothyronine deiodinase of rat liver is inhibited by extracts and secondary metabolites of plants. Hormone and Metabolic Research, 16(4), 188-192. doi: 10.1055/s-2007-1014739Axford, J., & O’Callaghan, C. (2004). Medicine (2nd ed.). Oxford, UK: Blackwell Publishing. Banasik, J.L. (2014). Disorders of endocrine function. In: Copstead, L-E, C., & Banasik, J.L. Pathophysiology (5th ed.) (pp. 799-815). St. Louis, MO: Elsevier. Barasi, M.E. (2003). Human nutrition: a health perspective (2nd ed.). London, UK: Hodder Arnold. Baskaran, K., Ahamath, B.K., Shanmugasundaram, K.R., & Shanmugasundaram, E.R.B. (1990). Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. Journal of Ethnopharmacology, 30(3), 295-305. doi: 10.1016/0378-8741(90)90108-6 Bartram, T. (1998). Bartram’s encyclopedia of herbal medicine. London, UK: Grace Publishers Beer, A.M., Wiebelitz, K.R., & Schmidt-Gayk, H. (2008). Lycopus europaeus (gypsywort): Effects on the thyroidal parameters and symptoms associated with thyroid function. Phytomedicine, 15(1-2), 16-22. Berkman, L.F., Leo-Summers, L., & Horwitz, R.I. (1992). Emotional support and survival after myocardial infarction: A prospective, population-based study of the elderly. Annals of Internal Medicine, 17(12), 1003-1009. doi: 10.7326/0003-4819-117-12-1003 Bone, K. (1994). Treating autoimmune disease: A phytotherapeutic perspective. Modern Phytotherapist, 1(1), 1-9. Bone, K., & Mills, S. (2013). Principles and practice of phytotherapy (2nd ed.). London, UK: Churchill Livingstone, Elsevier. Bove, M., Stansbury, J.E., & Romm, A. (2010). Endocrine disorders and adrenal support. In: Romm, A. Botanical Medicine for Women’s Health (pp.186-210) St. Louis, Missouri: Churchill Livingstone. Braun, L., & Cohen, M. (2015). Herbs and natural supplements: An evidence-based guide (4th ed.). Chatswood, Australia: Elsevier Health Sciences. Brock, C., Whitehouse, J., Tewfik, I., & Towell, T. (2014). American skullcap (Scutellaria lateriflora): A randomised, double-blind placebo-controlled crossover study of its effects on mood in healthy volunteers. Phytotherapy Research, 28(5), 692-698. doi: 10.1002/ptr.5044. Chevallier, A. (1994). Natural taste – herbal teas. Surrey, UK: Amberwood Publishing Ltd. Chevallier, A. (1996). The encyclopedia of medicinal plants. London, UK: Dorling Kindersley Ltd. Chevallier, A. (2008). Eyewitness companions: Herbal remedies. London, UK: Dorling Kindersley Ltd. Considine, R.V. (2013). Hypothalamus and the pituitary gland. In: Rhoades, R.A., & Bell, D.R. Medical physiology – principles for clinical medicine (4th ed.) (pp.604-620). Philadelphia, PA: Lippincott Williams & Wilkins. Cooley, K.,. Szczurko, O., Perri, D., Mills, E.J., Bernhardt, B., Zhou, Q., & Seely, D. (2009). Naturopathic care for anxiety: A randomised controlled trial ISRCTN78958974, PLoS ONE 4(8), 1-10. doi: 10.1371/journal.pone.0006628. Cooper, D. S. (2003) Hyperthyroidism. The Lancet, 362, 459-468. Emoto, M., & Nishizawa, Y. (2007). Diabetes mellitus and magnesium. In: Nishizawa, Y., Morii, H., & Durlach, J. (Eds.). New perspectives in magnesium research (pp. 187-212). London, UK: Springer. Davis, P.J., & Davis, F.B. (2001). Nontoxic goitre. In: Becker, K. L. (Ed.). Principles and practice of endocrinology and metabolism (3rd ed.) (pp. 366-373). Philadelphia, PA: Lippincott Willaims & Wilkins. Dowling, E.A., Redondo, D.R., Branch, J.D., Jones, S., McNabb, G., & Williams, M.H. (1996). Effect of Eleutherococcus senticosus on submaximal and maximal exercise performance. Medicine and Science in Sports and Exercise, 28(4), 482-489. Ellingwood, F. (1919). The American materia medica, therapeutics and pharmacognosy. Retrieved from: http://www.henriettes-herb.com/eclectic/ellingwood/index.html Eschbach. L., Webster, M., Boyd, J., McArthur, P., & Evetovich, T. (2000). The effect of Siberian ginseng (Eleutherococcus senticosus) on substrate utilization and performance during prolonged cycling. International Journal Of Sport Nutrition & Exercise Metabolism, 10(4), 444. Escott-Stump, S. (2002). Nutrition and diagnosis-related care (5th ed.). Baltimore, MD: Lippincott Williams & Wilkins. Felter, H.W., & Lloyd, J.U. (1898). King’s American dispensatory. Retrieved from http://www.henriettes-herb.com/eclectic/kings Gaffney, B.T., Hügel, H.M., & Rich, P.A. (2001). The effects of Eleutherococus senticosus and Panax gingseng on steroidal hormone indices of stress and lymphocyte subset numbers of endurance athletes. Life Sciences, 70(4), 431-442. doi:10.1016/S0024-3205(01)01394-7 Gropper, S., & Smith, J. (2012). Advanced nutrition and human metabolism. Hampshire, UK: Wadsworth Cengage Learning. Gross, L.S., Li, L., Ford, E.S., & Liu, S. (2004). Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: An ecologic assessment. American Journal of Clinical Nutrition. 79(5), 774-779. Haas, E.M. (1992). Staying healthy with nutrition. Berkeley, CA: Celestial Arts. Head, K.A., & Kelly. G.S. (2009). Nutrients and botanicals for treatment of stress: Adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Alternative Medicine Review, 14(2), 114. Hechtman, L. (2012). Clinical naturopathic medicine. Chatsworth, Australia: Elsevier. Hoffmann, D. (1997). The new holistic herbal. Dorset, UK: Element. Hoffmann, D. (2003). Medical herbalism: The science and practise of herbal medicine. Rochester, Vemont: Healing Arts Press. Kennedy, D.O., Little, W., & Scholey, A. (2004). Attenuation of laboratory-induced stress in humans after acute administration of Melissa officinalis (lemon balm). Psychosomatic Medicine, 66(4), 607-614. Kuo, J., Chen, K.W-C., Cheng, I-S., Tsai, P-H., Lu, Y-J., & Lee, N-Y. (2010). The effect of eight weeks supplementation with Eleutherococcus senticosus on endurance capacity and metabolism in human. Chinese Journal of Physiology, 53(2), 105-111. doi: 10.4077/CJP.2010.AMK018 Kumur, P., & Clark, M. (2002) Clinical medicine (5th ed.). Philadelphia, PA: Saunders. Longmore, M., Wilkinson, I.B., Baldwin, A., & Wallin, E. (2014). Oxford handbook of clinical medicine (9th ed.). New York, NY: Oxford University Press. mcDonald, j. (n.d.). Nettles, oats and you… Retrieved from: http://www.herbcraft.org/nettles%20oats%20and%20you.pdf McIntyre, A. (1999). The complete woman’s herbal. London, UK: Gaia Books Limited. McIntyre, A. (2005). Herbal treatment of children: Western and Ayurvedic perspectives. London, UK: Elsevier. Messaoudi, M., Lalonde, R., Violle, N., Javelot, H., Desor, D., Najdi, A., Bisson, J-F., Rougeot, C., Pichelin, M., Cazaubiel, M., Cazaubiel, J-M. (2010). Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. British Journal of Nutrition, 105(05), 775-764. doi: 10.1017/S0007114510004319 Mills, S. & Bone, K. (2000). Principles and practice of phytotherapy. London, UK: Churchill Livingstone. Mills, S., & Bone, K. (2008). The essential guide to herbal safety. London, UK: Churchill Livingstone, Elsevier. Mizokami, T., Wu, L.A., El-Kaissi, S., & Wall, J.R. (2004). Stress and thyroid autoimmunity. Thyroid, 14(12) 1047-55. doi: 10.1089/thy.2004.14.1047 Murray, M.T. (2012). Stress, anxiety, and insomnia: What the drug companies won’t tell you and your doctor doesn’t know. Coquitlam, British Columba, Canada: Mind Publishing Inc. Murray, M.T. (2014a). Natural support for stress, anxiety and insomnia. Retrieved from: http://doctormurray.com/natural-support-for-stress-anxiety-and-insomnia/ Murray, M.T. (2014b). Hypoglycaemia. Retrieved from: http://doctormurray.com/health-conditions/hypoglycemia/ Murray, M.T. & Pizzorno, J.E. (1999a). Hypothyroidism. In: Pizzorno, J.E., & Murray, M.T. Textbook of natural medicine (2nd ed.) (pp.1329-1334). London, UK: Churchill Livingstone. Murray, M.T. & Pizzorno, J.E. (1999b). Diabetes mellitus. In: Pizzorno, J.E., & Murray, M.T. Textbook of natural medicine (2nd ed.) (pp.1193-1218). London, UK: Churchill Livingstone. National Health Service (2014). Coeliac disease – treatment. Retrieved from: www.nhs.uk Neufeld, K-A., & Foster, J.A. (2009). Effects of gut microbiota on the brain: implications for psychiatry. Journal of Psychiatry & Neuroscience, 34(3), 230-231. Nussey, S.S., & Whitehead, S.A. (2001). Endocrinology: An integrated approach. Oxford, UK: BIOS Scientific Publishers Ltd. Panda, S., & Kar, A. (1998). Changes in thyroid hormone concentrations after administration of ashwagandha root extract to adult male mice. Journal of Pharmacy and Pharmacology, 50(9), 1065-8. doi: 10.1111/j.2042-7158.1998.tb06923.x Panda, S., & Kar, A. (1999). Withania somnifera and Bauhina purpurea in the regulation of circulating thyroid hormone concentrations in female mice. Journal of Ethnopharmacology, 67(2), 233-9. doi:10.1016/S0378-8741(99)00018-5 Park, S-H. (2006). Randomised clinical trials evaluating therapeutic influences of ornamental indoor plants in hospital rooms on health outcomes of patients recovering from sugery. Unpublished PhD thesis. Kansas State University. Retrieved from http://krex.k-state.edu/dspace/bitstream/handle/2097/227/Seong-HyunPark2006.pdf?sequence=1&isAllowed=y Park, S-H., & Mattson, R.H. (2008). Effects of flowering and foliage plants in hospital rooms on patients recovering from abdominal surgery. HortTechnology, 18(4), 563-568. Parsons, R., Tassinary, L.G., Ulrich, R.S., Hebl, M.R., & Grossman-Alexander, G. (1998). Journal of Environmental Psychology, 18(2), 113-139. doi: 10.1006/jevp.1998.0086 Pizzorno, J.E., Murray, M.T., Joiner-Bay, H. (2008). The clinician’s handbook of natural medicine (2nd ed.). St. Louis: MO: Churchill Livingstone. Pocock, G., & Richards, C.D. (2006). Human physiology the basis of medicine (3rd ed.). Oxford, UK: Oxford University Press. Pole, S. (2013). Ayurvedic medicine. London, UK: Singing Dragon Pratte, M.A., Nanavati, K.B., Young, V., & Morley, C.P. (2014). An alternative treatment for anxiety: A systematic review of human trial results reported for the Ayurvedic herb ashwaganda (Withania somnifera). Journal of Alternative and Complementary Medicine, 20(12), 901-908. doi: 10.1089/acm.2014.0177 Rosengren, A., Orth-Gomér, K., Wedel, H. & Wilhelmsen, L. (1993). Stressful life events, social support, and mortality in men born in 1933. British Medical Journal, 307, 1102. Rutledge, T., Reis, S.E., Olson, M., Owen, J., Kelsey, S.F., Pepine, C.J., Mankad, S., Rogers, W.J., Bairey Merz, C.N., Sopko, G., Cornell, C.E., Sharaf, B., & Matthews, K.A. (2004). Social networks are associated with lower mortality rates among women with suspected coronary disease: The National Heart, Lung, and Blood Institute-sponsored women’s ischemia syndrome evaluation study. Psychosomatic Medicine, 66(6), 882-8. Savignac, H.M., Corona, G., Mills, H., Chen, L., Spencer, J.P.E., Tzortzis, G., Burnet, P.W.J. (2013). Prebiotic feeding elevates central brain derived neurotrophic factor, N-methyl-d-aspartate receptor subunits and d-serine. Neurochemistry International, 63(8), 756–764. doi: 10.1016/j.neuint.2013.10.006 Schmidt, K., Cowan, P.J., Harmer, C.J., Tzortz, G., Errington, S., Burnet, P.W.J. (2014). Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology, 232(10), 1793-1801. doi: 10.1007/s00213-014-3810-0 Shanmugasundaram, E.R.B., Rajeswari, G., Baskaran, K., Kumar, B.R.R., Shanmugasundaram, K.R., & Ahmath, B.K. (1990). Use of Gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. Journal of Ethnopharmacology, 30(3), 281-294. doi:10.1016/0378-8741(90)90107-5 Shishtar, E., Sievenpiper, J. L., Djedovic, V., Cozma, A. I., Ha, V., Jayalath, V. H., Jenkins, D.J.A., Meija, S.B., de Souza, R.J., Jovanoski, E., & Vuksan, V. (2014). The effect of ginseng (the genus panax) on glycemic control: A systematic review and meta-analysis of randomized controlled clinical trials. PLoS ONE, 9(9), 1-11. doi: 10.1371/journal.pone.0107391 Stargrove, M.B., Treasure, J., & McKee, D.L. (2008). Herb, nutrient and drug interactions. St. Louis, MO: Mosby, Elsevier. Thomas, D., & Elliott, E.J. (2009). Low glycaemic index, or low glycaemic load, diets for diabetes mellitus (review). The Cochrane Collaboration. Retrieved from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006296.pub2/pdf Tillisch, K., Labus, J., Kilpatrick, L., Jiang, Z., Stains, J., Ebrat, B., Guyonnet, D., Legrain-Raspaud, S., Trotin, B., Naliboff, B., & Mayer, E.A. (2013). Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology, 144(7), 1394-1404. doi: http://dx.doi.org/10.1053/j.gastro.2013.02.043 Trickey, R. (2003). Women, hormones and the menstrual cycle. Crows Nest, Australia: Allen & Unwin. Tripathi, K.D. (2013). Essentials of medical pharmacology (7th ed.). London, UK: Jaypee Brothers Medical Publishers. Ulrich, R.S., Simons, R.F., Losito, B.D., Fiorito, E., Miles, M.A., & Zelson, M. (1991). Stress recovery during exposure to natural and urban environments. Journal of Environmental Psychology, 11(13), 201-230. doi: 10.1016/50272-49944(05)80184-7. Vanderpump, M.P. (2011). The epidemiology of thyroid disease. British Medical Bulletin, 99(1), 39-51. doi: 10.1093/bmb/ldr030 Vonhoff, C., Baumgartner, A., Hegger, M., Korte, B., Biller, A., & Winterhoff, H. (2006). Extract of Lycopus europaeus L. reduces cardiac signs of hyperthyroidism in rats. Life Sciences, 78(10), 1063-1070. doi: 10.1016/j.Ifs.2005.06.014 Weickert, M.O. & Pfeiffer, A.F.H. (2008). Metabolic effects of dietary fibre, consumption and prevention of diabetes. The Journal of Nutrition, 138(3), 439-442. Whitney, E., & Rolfes, S.R. (2013). Understanding nutrition (14th ed.). Stamford, CT: Cengage Learning. Winston, D., & Maimes, S. (2007). Adaptogens: herbs for strength, stamina, and stress relief. Rochester, Vermont: Healing Arts Press. Winterhoff, H., Sougens, H., & Kemper, F.H. (1983). Antihormonal effects of plant extract. Pharmacodynamic effects of lithospermum officinale on the thyroid gland of rats; comparison with the effects of iodide. Hormone and Metabolic Research, 15(10), 503-507. Winterhoff, H., Gumbinger, H.G., Vahlensieck, U., Kemper, F.H., Schmitz, H., & Behnke, B. (1994). Endocrine effects of Lycopus europaeus following oral application. Arzneimittel-Forschung, 44(1), 41-45. [Abstract] Wolfson, P., & Hoffmann, D.J. (2003). An investigation into the efficacy of Scutellaria lateriflora in healthy volunteers. Alternative Therapies, 9(2), 74-78. Yance, D.R. (2013). Adaptogens in Medical Herbalism. Rochester, Vermont: Inner Traditions / Bear & Co. Zimmermann, M.B. (2012). Iodine deficiency and endemic cretinism. In: Lewis, E.B., & Cooper, D.S. (Eds.). Wergner’s and Ingar’s the thyroid: A fundamental and clinical text (10th ed.) (pp. 217-241). London, UK: Lippincott Williams & Wilkins.
REFERENCES